This article was originally published by Prison Policy Initiative as “Addicted to punishment: Jails and prisons punish drug use far more than they treat it,” authored by Emily Widra.
Jails and prisons are often described as de facto mental health and substance abuse treatment providers, and corrections officials increasingly frame their missions around offering healthcare. But the reality is quite the opposite: people with serious health needs are warehoused with severely inadequate healthcare and limited treatment options. Instead, jails and prisons rely heavily on punishment, while the most effective and evidence-based forms of healthcare are often the least available.
This tension points to a crucial flaw in our nation’s reliance on criminalization: these institutions were never intended to be — and can never function as — healthcare providers. Efforts to reverse engineer them as such have proven ineffective, harmful, and financially wasteful, substituting medical best practices with moralizing and surveillance, from providing exclusively abstinence-based education to scanning and photocopying mail in a vain attempt to keep contraband out. This briefing builds on our past work about the unmet health needs of incarcerated people and the endless cycle of arrest for people who use drugs by compiling data on treatment availability versus drug-related punishment in jails and prisons across the country. We find that despite the lofty rhetoric, corrections officials punish people who use drugs far more than they provide them with healthcare.
Substance use disorders in jails and prisons far outpace rates in the general public
The prevalence of substance use disorders at every level of the criminal legal system points to an unavoidable fact: despite the deep unpopularity of the War on Drugs, our society still responds to substance use (and related crimes) as individual failures requiring punishment, rather than as a public health problem — and it’s not working.
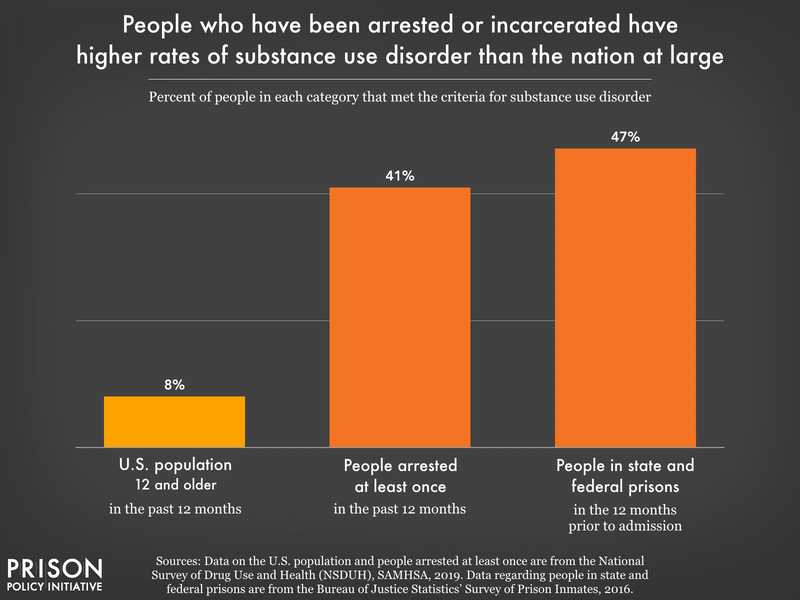
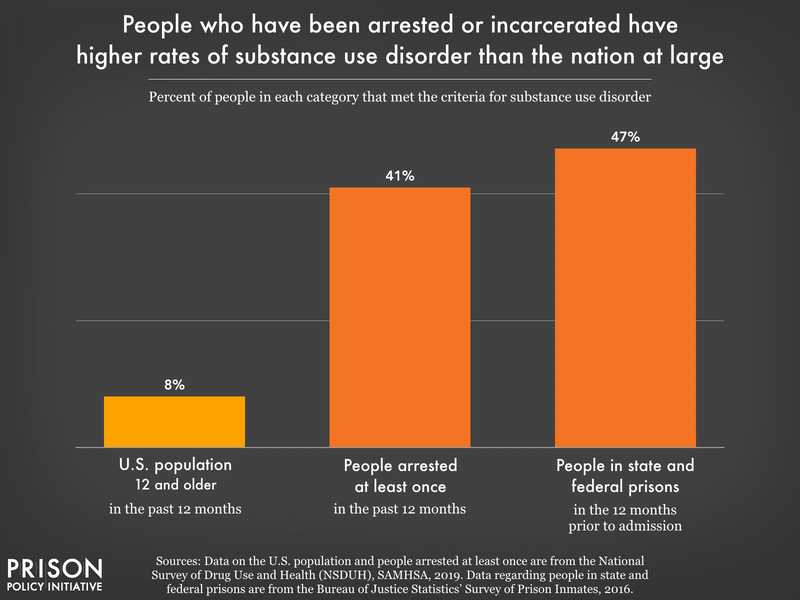
Nationally, approximately 8% of people met the criteria for substance use disorders in 2019, but such disorders are far more common among people who are arrested (41%) and people incarcerated in federal (32%) or state prisons (49%). This means that approximately three million people with substance use disorders are locked up in any given year: at least two million people with substance use disorders are arrested annually and about half a million people in state and federal prisons meet the criteria for such disorders at the time of their admission.
It’s difficult to see more granular trends in the data — such as the type of substances involved or the health outcomes related to these disorders — but we have some clues from nationally representative jail, prison, and mortality data.
Jails. In 2019, only 64% of all people admitted to jail each month were screened for opioid use disorder, but of those people, about 15% met the criteria for opioid use disorder. It’s likely that in jails where not everyone is screened on admission, people have similarly high rates of opioid use disorder, given the widespread extent of the opioid crisis. Because we cannot see the full picture through screenings alone, it’s useful to look at mortality data as well. More than 15% of jail deaths in 2019 were attributed to drug or alcohol intoxication (overdose), a significant increase from 4% in 2000 and 7% in 2009.
Prisons. Many people who use drugs and need care are arrested and jailed over and over until, finally, one event lands them in prison. We estimate that more than 578,000 people (47%) in state and federal prisons in 2022 had a substance use disorder in the year prior to their admission. And while the mortality rates for drug and alcohol intoxication are lower in prisons than in jails, almost 7% of all deaths in state prisons in 2019 were due to drug or alcohol intoxication, compared to less than 2% in 2009. Meanwhile, in 2019, only 4% of all adult deaths in the U.S. were attributed to drugs or alcohol. All of these measures point to much higher rates of substance use disorders in prisons and jails compared to the total population.
Treatment options for opioid use disorder are scarce in jails and prisons
Not every person who uses substances needs or wants treatment, but it is imperative that evidence-based, quality healthcare options be made available for those who do — regardless of their involvement in the criminal legal system. For people with opioid use disorder, this can include psychosocial treatment (including counseling), medication-assisted treatment (MAT), and self-help groups. In correctional settings, the availability of such options pales in comparison to the level of need.
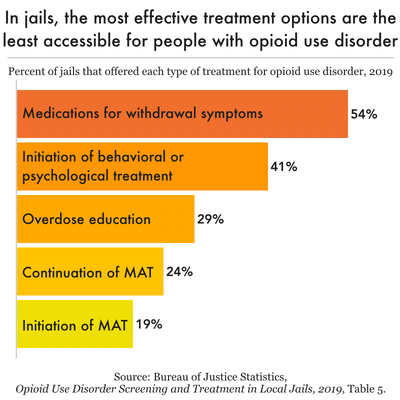
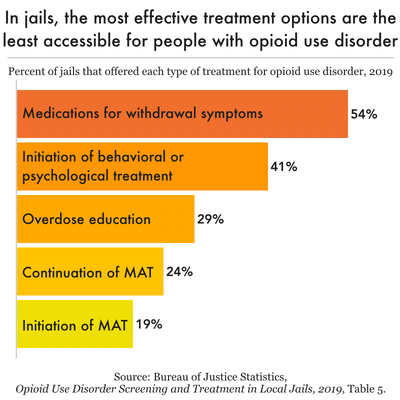
Jails. Of the nearly 3,000 local jails across the country, less than two-thirds (63%) screen people for opioid use disorder when they are admitted. Only half (54%) provide medications for people experiencing withdrawal. An even smaller percentage of jails — 41% — provide behavioral or psychological treatment, and 29% provide education about overdose. In fact, the most effective treatment — medication-assisted treatment (MAT) — is the least commonly provided: just 24% of jails continue MAT for people already engaged in treatment while only 19% initiate MAT for those who are not.
Quality medical interventions for people that use opioids are especially urgent in jails because of the rapid and acute risk of withdrawal. Over half a million people entering jails across the country each year are experiencing or at risk of this life-threatening medical event. Importantly, the percentage of people admitted to jail who receive treatment for opioid withdrawal varies significantly between states, which likely reflects differences in both opioid use and availability of treatment. For instance, over 15% of people admitted to jails in June 2019 in four states — New Hampshire, New Jersey, Pennsylvania, and Washington — were treated for opioid withdrawal, compared to less than 1% of admissions in seven other states.
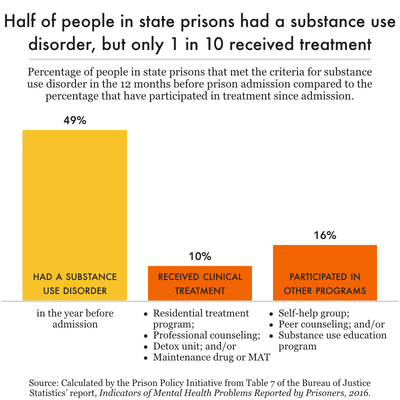
Prisons. Most state and federal prisons (81%) offered some “drug or alcohol dependency, counseling, or awareness programs” in 2019, but among people in state prisons with a substance use disorder, only 10% had received clinical treatment in the form of a residential treatment program, professional counseling, detoxification unit, or MAT. This suggests the “drug or alcohol programming” available in prison facilities is primarily self-help or peer-based.
Jails and prisons are often described as de facto mental health and substance abuse treatment providers, and corrections officials increasingly frame their missions around offering healthcare.1 But the reality is quite the opposite: people with serious health needs are warehoused with severely inadequate healthcare and limited treatment options. Instead, jails and prisons rely heavily on punishment, while the most effective and evidence-based forms of healthcare are often the least available.
This tension points to a crucial flaw in our nation’s reliance on criminalization: these institutions were never intended to be – and can never function as – healthcare providers. Efforts to reverse engineer them as such have proven ineffective, harmful, and financially wasteful, substituting medical best practices with moralizing and surveillance, from providing exclusively abstinence-based education to scanning and photocopying mail in a vain attempt to keep contraband out. This briefing builds on our past work about the unmet health needs of incarcerated people and the endless cycle of arrest for people who use drugs by compiling data on treatment availability versus drug-related punishment in jails and prisons across the country. We find that despite the lofty rhetoric, corrections officials punish people who use drugs far more than they provide them with healthcare.
Substance use disorders in jails and prisons far outpace rates in the general public
The prevalence of substance use disorders at every level of the criminal legal system points to an unavoidable fact: despite the deep unpopularity of the War on Drugs, our society still responds to substance use (and related crimes) as individual failures requiring punishment, rather than as a public health problem — and it’s not working.
Nationally, approximately 8% of people met the criteria for substance use disorders in 2019,2 but such disorders are far more common among people who are arrested (41%) and people incarcerated in federal (32%) or state prisons (49%). This means that approximately three million people with substance use disorders are locked up in any given year: at least two million people with substance use disorders are arrested annually and about half a million people in state and federal prisons meet the criteria for such disorders at the time of their admission.3
It’s difficult to see more granular trends in the data – such as the type of substances involved or the health outcomes related to these disorders – but we have some clues from nationally representative jail, prison, and mortality data.
Jails. In 2019, only 64% of all people admitted to jail each month were screened for opioid use disorder, but of those people, about 15% met the criteria for opioid use disorder. It’s likely that in jails where not everyone is screened on admission, people have similarly high rates of opioid use disorder, given the widespread extent of the opioid crisis.4 Because we cannot see the full picture through screenings alone, it’s useful to look at mortality data as well. More than 15% of jail deaths in 2019 were attributed to drug or alcohol intoxication (overdose), a significant increase from 4% in 2000 and 7% in 2009.
Prisons. Many people who use drugs and need care are arrested and jailed over and over until, finally, one event lands them in prison. We estimate that more than 578,000 people (47%) in state and federal prisons in 2022 had a substance use disorder in the year prior to their admission.5 And while the mortality rates for drug and alcohol intoxication are lower in prisons than in jails, almost 7% of all deaths in state prisons in 2019 were due to drug or alcohol intoxication, compared to less than 2% in 2009. Meanwhile, in 2019, only 4% of all adult deaths in the U.S. were attributed to drugs or alcohol.6 All of these measures point to much higher rates of substance use disorders in prisons and jails compared to the total population.
Treatment options for opioid use disorder are scarce in jails and prisons
Not every person who uses substances needs or wants treatment, but it is imperative that evidence-based, quality healthcare options be made available for those who do — regardless of their involvement in the criminal legal system. For people with opioid use disorder, this can include psychosocial treatment (including counseling), medication-assisted treatment (MAT), and self-help groups. In correctional settings, the availability of such options pales in comparison to the level of need.
Jails. Of the nearly 3,000 local jails across the country, less than two-thirds (63%) screen people for opioid use disorder when they are admitted. Only half (54%) provide medications for people experiencing withdrawal. An even smaller percentage of jails — 41% — provide behavioral or psychological treatment, and 29% provide education about overdose. In fact, the most effective treatment — medication-assisted treatment (MAT) — is the least commonly provided: just 24% of jails continue MAT for people already engaged in treatment while only 19% initiate MAT for those who are not.
Quality medical interventions for people that use opioids are especially urgent in jails because of the rapid and acute risk of withdrawal. Over half a million people9 entering jails across the country each year are experiencing or at risk of this life-threatening medical event.10 Importantly, the percentage of people admitted to jail who receive treatment for opioid withdrawal varies significantly between states, which likely reflects differences in both opioid use and availability of treatment.11 For instance, over 15% of people admitted to jails in June 2019 in four states – New Hampshire, New Jersey, Pennsylvania, and Washington – were treated for opioid withdrawal, compared to less than 1% of admissions in seven other states.12
Prisons. Most state and federal prisons (81%) offered some “drug or alcohol dependency, counseling, or awareness programs” in 2019, but among people in state prisons with a substance use disorder, only 10% had received clinical treatment in the form of a residential treatment program, professional counseling, detoxification unit, or MAT.13 This suggests the “drug or alcohol programming” available in prison facilities is primarily self-help or peer-based.14
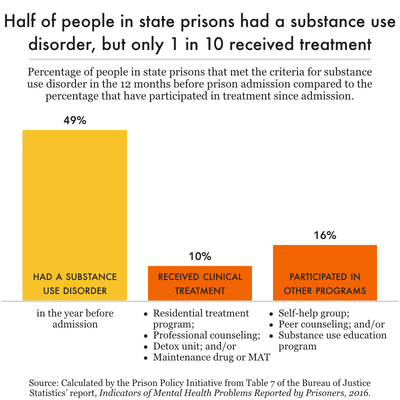
Unfortunately, MAT is the least common treatment in prisons: only 1% of people with substance use disorders in state and federal prisons reported receiving MAT at any point since their admission. In North Carolina, for example, over 9,000 people admitted to state prisons in Fiscal Year 2021-22 (78% of everyone screened during intake) met the criteria for needing intermediate or long-term substance use treatment, but the clinical director of the Alcoholism and Chemical Dependency Programs reports that they are only able to treat 3,000 cases each year. The state launched a MAT pilot program in 2021, and as of January 2024, only 213 enrollees have received medications prior to release from prison.
Even when correctional facilities do offer necessary treatments, their one-size-fits-all approaches can be limiting, overlooking the specific needs of different populations. For example, women in prison are often expected to participate in treatment programs originally designed for men. Advocates report that because “there are fewer incarcerated women than men… there are fewer programs available for women serving time. If support is available, it is not always effective.”
Ineffective and punitive responses to drug use in correctional facilities
Correctional facilities’ preference for punishment does very little to actually reduce drug use and overdoses. It’s not just that officials fail to provide evidence-based healthcare–they actively ignore evidence that punitive drug interdiction policies like mail scanning and visitation restrictions are ineffective and counterproductive, too.
Mail scanning. Prisons and jails are increasingly diverting incoming letters, greeting cards, and artwork, making photocopies or digital scans of them, and delivering those inferior versions to recipients.15 Administrators claim this practice will stem the flow of contraband — primarily, drugs — into their facilities, but there is no solid evidence to date that mail scanning has this intended effect.16 In addition to the emotional consequences and needless exploitation inherent in mail scanning, these practices result in long mail delays and the disruption of correspondence-based nonprofits, education programs, and ministries.
There are numerous examples of mail scanning failing to produce any meaningful reduction in drug use or overdoses in prisons across the country:
- Pennsylvania: After instituting mail scanning, the percentage of incoming mail that the Department of Corrections reported as “tainted” only decreased by 0.1% over the course of a year. As of 2023, the rate of positive drug tests in Pennsylvania prisons is now almost 3 times higher than it was before the policy was introduced.
- Missouri: In Missouri state prisons, the average number of overdoses per month increased from 34 to 39 after mail scanning was introduced in July 2022.
- Virginia: Every year since the Virginia Department of Corrections began mail scanning in 2017, there have been more overdoses than in the year prior to instituting mail scanning (even while the state’s incarcerated population declined during the COVID-19 pandemic).
- New Mexico: After a mail scanning policy went into effect in February 2022, a report on the Corrections Department from the state’s Legislative Finance Committee highlighted a nearly two-percentage point increase in positive random drug test results from Fiscal Year 2021 to Fiscal Year 2022 – almost doubling the positivity rate. This essentially “reverse[d] three years of reduced drug use” in the prison system, and the report authors noted that the mail scanning policy “does not appear to have reduced drug use” during the study period.
In fact, several prison systems seem to actively ignore the lack of evidence supporting mail scanning as a drug interdiction effort. The federal Bureau of Prisons has increasingly adopted mail scanning policies, reportedly following a letter from Pennsylvania congressional representatives “urg[ing] the BOP to follow Pennsylvania’s lead,” and such policies are now in place in almost every federal facility.
Visitation restrictions. There are a variety of policies in jails and prisons that restrict visitation and administrators often defend them as anti-contraband (i.e., anti-drug) initiatives. For example, in Virginia, some of these policies have included requiring visitors to change into state-issued jumpsuits without pockets, limiting approved visitor lists to 10 people, millimeter wave body scanners, and banning feminine hygiene products for visitors.17 In Washington, the latest state budget proposal betrays the state’s biases in responding to drugs in prisons: it includes $4.7 million for MAT in prisons, which is only about half of the funding it would take to meet the needs of people in custody. At the same time, the Department requested $6.5 million for body scanner staff and operations, and the budget proposal offers even more than they asked for: $7.9 million. Incarcerated people routinely face humiliating search practices – including strip searches – following visitation, but considering the prevalence of drug use inside prisons and jails, these tactics do not appear to have made a meaningful impact.
Doubling down on failure: misunderstanding drug use inside
Prison and jail administrators often cite contraband medication as the primary reason for restricting access to MAT. While “diversion” of medications18 like buprenorphine can occur in prisons and jails, there are simple, proven diversion prevention strategies that any facility offering MAT could institute, whether they are correctional facilities or community health centers. 19 We know that generally, “illicitly obtained” buprenorphine is most often used to self-treat opioid withdrawal when treatment is not available or has been denied. While there is much concern regarding diversion, an extensive analysis of Bureau of Justice Statistics’ mortality data from 2000-2013 revealed no overdose or death reports mentioning buprenorphine or Suboxone, consistent with previous research on New York City non-incarcerated overdose fatalities. It is clear that – just like in the community – the proven benefits of MAT outweigh the perceived risks of diversion.
Consistent with their punitive approach to drugs, many corrections officials enforce serious sanctions for positive drug tests, medication diversion, and non-fatal overdoses. Sanctions for drug use in prisons can include solitary confinement, denied visitation, 20 delayed parole hearings, loss of “good time,” reduced access to programming, facility transfers, reclassification, and fines.21 There is, unsurprisingly, no evidence that these disciplinary policies actually reduce drug use behind bars. However, it’s easy to imagine how such approaches create a dynamic in which people hide their drug use and engage in riskier, deadlier behaviors. The culture fostered by punishment does not actually address drug use — it just makes it more dangerous.
Public health research has long been clear that punishing addiction does not actually help address substance use disorders, and there is no reason that it would work in jails and prisons. People who need mental health and substance use treatment are better served in voluntary, non-carceral, clinical treatment settings.
Overdose interventions and deaths
Jail and prison administrators are right to be concerned about drug overdoses behind bars. Overdose deaths are preventable and substance use disorders are treatable, but in 2019, more than 400 people in jails and prisons died of drug or alcohol intoxication.22
Jails. In response to overdoses, some local jails have increased the availability of naloxone (an opioid overdose reversal medication also known by the brand name “Narcan”). In Maine, correctional staff in some facilities now carry naloxone on their belts rather than in a locked first aid kit. In New York City, all housing areas are required to have naloxone available.
Some jails have gone a step further: in San Diego County, the staff and people in custody have access to naloxone throughout the jail facility. In Los Angeles County jails and the Louisville Metro Department of Corrections jail in Kentucky, staff and incarcerated people have access to naloxone and receive training on how to administer it. The benefits of this dual approach cannot be overstated: in a single day in Los Angeles, two overdoses were reversed when incarcerated people administered naloxone and, over the course of a year, incarcerated people in the Louisville jail dispensed naloxone successfully to at least 24 people who had overdosed in the facility.
Prisons. The rates of death from drug or alcohol intoxication may be lower in prisons than in local jails, but they are still a serious – and growing – problem: from 2001 to 2019, the percentage of state prison deaths attributed to drug and alcohol intoxication increased from 1.2% to 6.6%. A September 2022 directive from the New York State Department of Corrections and Community Supervision requires correctional staff to administer naloxone as well as provide first aid and CPR as necessary, and includes a requirement for each facility to institute a procedure to make naloxone more accessible to staff. In Oklahoma, the State Department of Mental Health and Substance Abuse Services reported that naloxone is available “on every unit” in state prisons, and future initiatives where “every CO will have Narcan on them” are expected as of May 2023.
Making naloxone physically present in correctional facilities is a good first step, but it’s not enough. In April 2023, reporting from Filter detailed that, while correctional staff in Washington Department of Corrections facilities have access to naloxone, many are not properly trained. When interviewed, two correctional officers – incorrectly – told the reporter that “Narcan…doesn’t work on fentanyl.” The Filter story cites at least one Department of Corrections report of an overdose scene where staff were unable to locate, and were unsure how to administer, naloxone. As long as the criminal legal system continues to target and incarcerate people who use drugs, screening new admissions for opioid use, training staff and incarcerated people to use naloxone, and making naloxone available throughout facilities are the least these institutions could do.
Making reentry safer for people who use drugs
There are two crucial interventions that every jail and prison should offer upon release: free access to naloxone and appropriate, timely referrals to community-based MAT for people who received treatment while incarcerated. Yet less than one-third of local jails and far fewer prison systems offer either.
Naloxone. While naloxone is relatively inexpensive and easy to administer, in 2019, only 25% of jails provided naloxone to people being released. However, in the years following the 2019 survey, media coverage reveals that many jails – including those in Louisville, Kentucky, and Kershaw County, South Carolina – have added free naloxone vending machines near the facility exits.
In 2020, the California Department of Corrections and Rehabilitation began providing free naloxone kits and training to people preparing for release from prison. By July 2022, 95% of people released from California state prisons had received the kits and training. A handful of other prison systems have publicized similar efforts to provide naloxone on release but with little accompanying data on the success of their projects. For example, the Indiana Department of Corrections announced an initiative in 2020 to offer people released from prison the “opportunity to leave with Naloxone,” but there is little evidence available on the outcome of this program. Meanwhile, some states remain hostile to this very simple and effective intervention. In 2023, Oklahoma Governor Kevin Stitt vetoed a bill that would allow prisons to give Narcan to people upon release.23
Community referrals for MAT. In 2019, only 28% of local jails provided a community link to MAT on release. Jails need to partner with their local public health agencies to identify community-based MAT providers for people returning home. For people who started or continued MAT while in jail, uninterrupted access to that treatment is vital. These efforts must include support in navigating the often-complicated health insurance landscape. In 2019, 27% of people on parole and 23% of people who had been arrested at least once in the past year reported having no health insurance coverage. People leaving jail or prison who need MAT must have primary care providers and Medicaid, Medicare, or other health insurance set up prior to release.
Recommendations
It is clear that the criminal legal system is not suited to the task of acting as the de facto mental health and substance abuse treatment provider many claim it to be. There are at least a few areas ripe for intervention to improve this situation: reducing the number of people with substance use disorders entering the criminal legal system, instituting evidence-based practices in correctional facilities that actually reduce the risk of drug overdoses, and expanding treatment availability inside jails, prisons, and during reentry.
Prevent people with substance use disorders from entering the criminal legal system:
- Address the social determinants of health and substance use. In order to reduce the flow of people with substance use disorders into jails and prisons, communities must prioritize housing, physical and mental healthcare, employment, and education. Increased funding for community-based drug treatment and other social services are crucial.
- Decriminalize drug use. People should not be confined in jails or sentenced to incarceration for drug possession, drug checking supplies, or drug paraphernalia. Harm reduction efforts like clean syringe exchanges, overdose prevention centers, safety-focused education programs, and regulating the drug supply will more effectively – and humanely – reduce overdose risk among people who use drugs.
Institute effective, nonpunitive responses to drug use behind bars:
- Screen for all substance use and mental health disorders. All admissions to prisons and jails should be screened for active substance use, substance use disorders, and mental health conditions.
- Avoid punishments and restrictions as responses to drug use, particularly when there is no evidence that they meaningfully impact consumption and overdose. Reflexively restricting meaningful contact and relationships under the guise of drug prevention is especially harmful and counterproductive. This inevitably requires divesting from ineffective practices like mail scanning, canine drug detection, and electronic scanning equipment for visitation. There should be more focus on treatment than punishment for incarcerated people who struggle with addiction.
- Invest in comprehensive MAT in jails and prisons including professional, clinical counseling, the availability of all MAT drugs, referrals to community providers upon release, and support reestablishing health insurance during reentry.
Expand treatment availability for substance use disorders:
- Treatment participation must be voluntary in jail, prison, and the community. When treatment is involuntary or coerced, when people are re-incarcerated for positive drug tests, or when they’re disqualified from participation in diversion programs based on their history of substance use, treatment is less effective. Instead, as the Drug Policy Alliance recommends, treatment should always be voluntary, involve clinicians rather than law enforcement, incorporate positive incentives, and use gold-standard medication and other practices.
- Treatment should begin as soon as possible. Any kind of treatment for substance use disorders and mental health conditions cannot be limited to the weeks or months leading up to release from jail or prison.
- Treatment requires informed consent. Healthcare providers should seek out informed consent from all individuals who are eligible for MAT and they must have access to all treatment options.
Substance use disorder treatment — as handed down by the criminal legal system — is not working as advertised. Jails and prisons are not healthcare institutions and their mandate for punishment makes patient-centered care impossible and health outcomes worse. Instead, the United States desperately needs healthcare infrastructure that can support people who use drugs outside of carceral settings. While corrections officials request further investments under the guise of treatment, the stigma, isolation, and punishment that helped foment the present crisis persist. Our communities cannot punish their way out of public health crises, but as long as policymakers insist on incarcerating people with substance use disorders, they need to at least provide evidence-based care to those who want and need it.
Footnotes
- In December 2023, for example, the Arapahoe County (Colorado) Sheriff justified an expected $46 million jail expansion project by claiming the jail needs more space to provide healthcare services to confined people: “The needs of the people that we are in custody of have changed,” Brown said. “We’re not warehousing individuals anymore. We’re treating them.” ↩
- The National Survey of Drug Use and Health (NSDUH) surveys a nationally representative sample of people aged 12 and older. For the purposes of this analysis, we chose to use data collected in the 2019 NSDUH rather than the more recent 2020 survey results. In the 2020 NSDUH report, the authors cautioned that “care must be taken when attempting to disentangle the effects on estimates due to real changes in the population (e.g., the coronavirus disease 2019 [COVID-19] pandemic and other events) from the effects of these methodological changes.” Because of this warning, we elected to use 2019 NSDUH so that our results could be better compared over time and to the available criminal legal system data, which is primarily from 2016-2019. Researchers updating our work in the future, however, should note one important methodological change occurred in 2020: the 2020 survey was the first year in which substance use disorders were evaluated using criteria defined in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-V), as opposed to the 4th edition (DSM-IV). ↩
- In 2016, 47% of people in state and federal prisons met the criteria for substance use disorders prior to admission. Applying this percentage to the 2022 combined state and federal prison population of 1,230,100, we estimate that at least 578,147 people met substance use disorder criteria prior to admission. ↩
- In small jails (holding less than 50 people), only 36% of admissions were screened, but they still had 15% of people screening positive. In jails with 50-250 people, about half (51%) of admissions were screened, and the percentage screening positive was higher: 19-22%. The largest jail jurisdictions (holding 1,000+ people) had higher screening rates but lower rates of positive screenings, which suggests that some smaller jurisdictions may only be screening people whom they suspected of having an opioid use disorder. ↩
- In 2016, 47% of people in state and federal prison met the criteria for substance use disorders in the year prior to admission. Applying this percentage to the 2022 prison population of 1,230,100, we estimate that 578,147 people met substance use disorder criteria in the year prior to admission. ↩
- Centers for Disease Control and Prevention, National Center for Health Statistics. National Vital Statistics System, Mortality 2018-2021 on CDC WONDER Online Database, released in 2021. Data are from the Multiple Cause of Death Files, 2018-2021, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. Query criteria included ages 18 and older, drug- or alcohol-induced causes of death, and data for 2019. ↩
- Other substance use disorders can be addressed with MAT. For example, there are medications for alcohol use disorder (MAUD) that include acamprosate, disulfiram, and naltrexone. However, for the purposes of this briefing, we are focused on MAT for opioid use disorder (also known as MOUD) as there is little to no information about MAUD in prisons and jails. ↩
- A 2019 study based on interviews with state prison representatives from 21 states found that only 7% of prisons in these states offered all three medications. The most commonly provided was naltrexone, which was provided in 36% of prisons in the survey. While any MAT is better than no treatment, there is some evidence that people who receive buprenorphine have significantly lower risk of opioid overdoses than those who receive naltrexone. ↩
- This estimate is calculated based on the 5% of all jail admissions in June 2019 that were treated for opioid withdrawal with medications and the 894,030 jail admissions in June 2019. This is inevitably an undercount, as not all people admitted to jail in active withdrawal are provided with medical care. If 5% of the people admitted to jail in a single month were treated for withdrawal, that means that at least 536,400 people entering jails in 2019 met the criteria for medical intervention for opioid withdrawal. ↩
- Deaths associated with alcohol or drug withdrawal (which can be lethal, especially among people with multiple health concerns) are not included in the “drug or alcohol intoxication” deaths reported in the Bureau of Justice Statistics mortality data, but rather these deaths are most often included in the counts of deaths attributed to “illness” or “other,” according to the Bureau of Justice Assistance. In an extensive analysis of Bureau of Justice Statistics’ mortality data from 2000-2013, researchers found that drug and alcohol related deaths in jails were likely significantly underreported and that there were “roughly 50% more deaths involving drugs or alcohol than previously estimated,” including at least 87 withdrawal-related jail deaths. ↩
- While no region or state in the nation is immune to the opioid crisis, we do know that there is significant variation in opioid use, overdose rates, and access to treatment across the country. ↩
- Kansas, Nebraska, North Dakota, South Dakota, Alaska, Idaho, Wyoming treated less than 1% of statewide jail admissions for opioid withdrawal in June 2019. ↩
-
In the Survey of Prison Inmates, 2016, these treatment options are defined as follows:
- Detoxification: An alcohol or drug detoxification unit where prisoners spent up to 72 hours to “dry out.”
- Residential program: An alcohol or drug program in which prisoners lived in a special facility or unit designated for treatment.
- Counseling and therapy: Counseling sessions with a trained professional while not living in a special facility or unit.
- Self-help group: Includes peer counseling programs, such as Alcoholics Anonymous, Cocaine Anonymous, or Narcotics Anonymous, and other forms of self-help groups.
- Education program: An education or awareness program “explaining problems with alcohol or drugs in any setting.”
- Medication-assisted treatment: A maintenance drug, such as methadone, disulfiram, or naltrexone, that is used to “cut a high or make you sick.”
- There is nothing inherently wrong with offering self-help, 12-step, or peer-counseling programming in prisons. It is only problematic when facilities only offer these types of interventions to people eligible for MAT and/or other clinical treatments ↩
- Paper mail is often the cheapest and most-used form of communication for people in prison and their loved ones. ↩
- This practice of mail scanning, either performed at the facility or off-site using a third-party vendor, strips away the privacy and the sentimentality of mail, which is often the least expensive and most-used form of communication between incarcerated people and their loved ones. Among other jurisdictions, administrators in the federal Bureau of Prisons, the Pennsylvania Department of Corrections, the New York City Department of Correction, the Virginia Department of Corrections, and the Missouri Department of Corrections claimed that mail scanning policies were instituted to reduce drug contraband. ↩
- In 2018, the Virginia Department of Corrections banned visitors from wearing tampons or menstrual cups because of “many instances” of drug smuggling. The Department never reported a count of these instances, and eventually reversed this unjustified and invasive policy in 2019 following significant pushback. ↩
- Drug diversion, according to the Colorado Department of Public Health & Environment, occurs when a medication is taken for use by someone other than whom it is prescribed or for an indication other than what is prescribed. ↩
- In addition, there are other significant avenues through which drugs flow into prisons – including via correctional officers. The federal Bureau of Prisons reported on staff bringing drugs into facilities as early as 2003. More recently, there have been substantiated reports of correctional officers bringing drugs into an Ohio jail, a federal facility in Atlanta, and New York City jails. A 2018 report from NYC’s Department of Investigation revealed that an undercover investigator smuggled in scalpels, marijuana, and Suboxone into the Manhattan and Brooklyn Detention Centers, passing through “all screening checkpoints at both facilities without being manually searched,” even after triggering multiple metal detection devices. A 2023 report from the Office of the Inspector General in California reported that while all California Department of Corrections and Rehabilitation (CDCR) staff and contractors are supposed to be searched, these searches are often inadequate. The report also cites an agreement between the CDCR and the California Correctional Peace Officers Association that stipulates “enhanced inspections will not include a hands-on, physical search of an employee’s person or the use of canines.” ↩
- In-person visitation is one of the most important factors for maintaining family and community support through incarceration and setting up individuals for successful reentry. ↩
- All prison and jail systems have disciplinary responses to drug use. Some examples can be found in the 2022 Office of the Inspector General’s report, Investigation of New York State Department of Corrections and Community Supervision Incarcerated Individual Drug Testing Program, Kyle Ruggeri’s 2019 reporting on his time spent in solitary confinement while in withdrawal in New York State prison, and recent reporting on a class-action lawsuit against the Washington Department of Corrections. For links to prison system discipline policies for state prisons, the District of Columbia Department of Corrections, and the federal Bureau of Prisons, see our Disciplinary Policies collection. ↩
- The most recent iteration of the Bureau of Justice Statistics’ Mortality in Local Jails and State and Federal Prisons series covers deaths occurring in 2019. This is the most recent national data on cause of death in correctional facilities. ↩
- At the same time, Governor Stitt also vetoed a bill authorizing hospitals to give Narcan to people with opioid use disorders upon discharge. ↩
This article was originally published by Prison Policy Initiative as “Addicted to punishment: Jails and prisons punish drug use far more than they treat it,” authored by Emily Widra